38% Bogged Down by Admin Bloat—Streamline in 3 Easy Steps
A new report from Physicians Practice lays out the stark reality for today’s healthcare organizations: 2025 is shaping up to be one of the most operationally strained years in recent memory.
According to their latest poll:
58% of clinics cite payer friction—especially prior authorizations—as their #1 issue
56% report ongoing staffing shortfalls
42% are struggling with rising operational costs
And 38% are buried in administrative bloat
If you’re running a clinic, you’re likely feeling the pressure on every front: delays from payers, burnout from staff turnover, and shrinking margins from inflation and reimbursement cuts. And buried under it all is the administrative overload that steals time, saps morale, and chips away at your team’s efficiency.
Let’s talk about how to get some of that time—and peace of mind—back.
Step 1: Automate Where You Can
Many of the repetitive tasks still being handled manually—like vitals checks, routine symptom monitoring, and chronic care check-ins—can be offloaded to automated systems. Doing so helps eliminate duplicate documentation, reduces manual logging, and creates more consistent patient follow-through.
Practices using automated care protocols report 20–30% fewer manual chart entries and a measurable drop in missed patient flags.
Step 2: Simplify Team Communication
Fragmented communication channels—between EHRs, texts, voicemails, and task apps—only amplify staff stress. A centralized communication tool allows real-time updates, consolidated care plans, and reduces the chance of critical tasks slipping through the cracks.
Annals of Internal Medicine reports the average physician now spends 16 minutes per patient managing the EHR—most of it non-clinical.
Step 3: Rethink Follow-Up with Remote Monitoring
Instead of chasing down patients for check-ins, proactive clinics are deploying Remote Patient Monitoring (RPM). RPM allows staff to track vitals and symptoms passively in real time, with built-in alerts
when something goes off track. That means fewer calls, faster response time, and less stress on staff.
The RPM Edge: Results You Can Measure
RPM isn’t just a solution for continuity—it’s an engine for time recovery and better care.
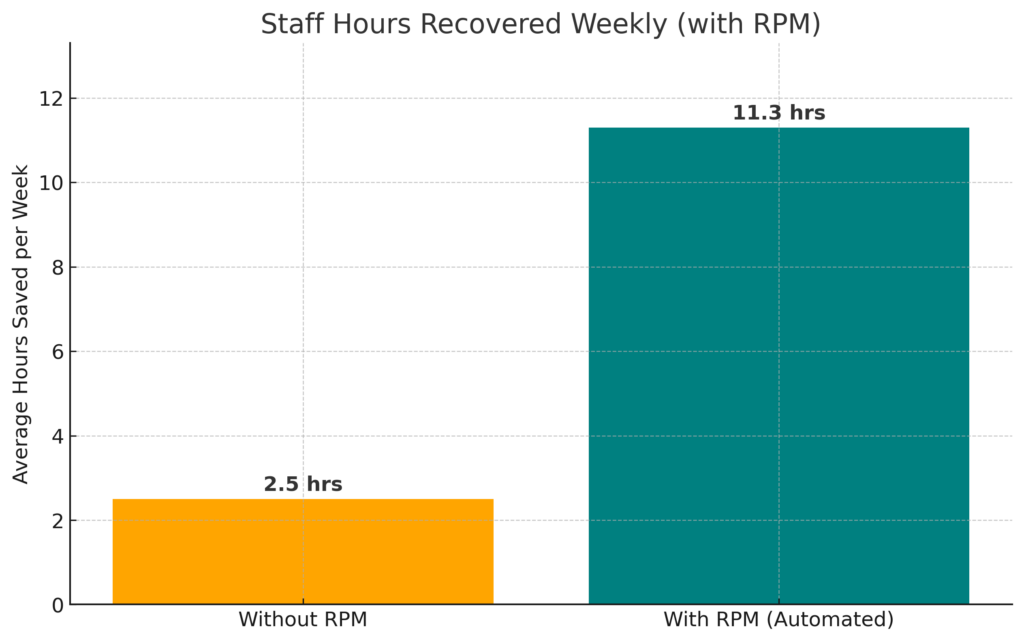
Source: Journal of Ambulatory Care Management, Q1 2025
Follow-Up Completion Rates
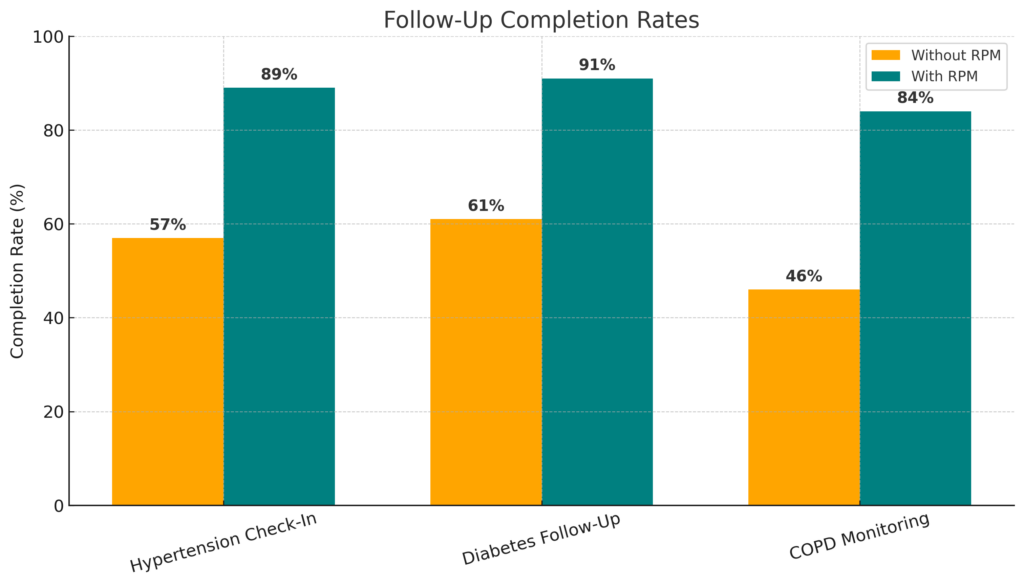
Source: Remote Care Trends Report, April 2025
Why This Matters More Than Ever
The prior authorization workload alone now eats up nearly two business days per physician each week (AMA, 2025). Meanwhile, medical assistants are harder to hire than ever, and the reimbursement landscape continues to contract—down another 2.83% in 2025 under Medicare.
When 38% of practices say administrative bloat is a top concern, and only 2% are actively investing in new technology like AI, the gap becomes clear: many clinics need a smarter system but lack the bandwidth to implement one.
The Fix Starts Small
You don’t need to overhaul your clinic overnight.
You just need tools that reduce the noise.
Platforms built around remote care delivery—like RPM and CCM—can automate the repetitive, flag the risky, and keep patients engaged without straining your team.
Let us know if you’d like help mapping out a pilot strategy that fits your current workflows
